猴痘1例及文献复习
文章导读:了解猴痘的临床表现、检测及诊断方法。方法 对近期确诊的1例猴痘患者临床及实验室资料进行分析,并对国内外报道相关病例资料进行回顾。结果 此病例为43岁男性患者,发热2~3 d后在阴阜及阴茎干出现红斑丘疹,继而形成脓疱,脓疱破溃后局部溃疡。患者既往有梅毒史。皮肤科检查:右侧阴阜部红肿明显,红肿部位可见结痂脓疱,阴茎包皮及冠状沟各1处结痂脓疱。皮损、血液、咽喉拭子标本猴痘病毒核酸检测阳性,利用 Nextclade 工具(参考基因组 NC_063383.1)对该序列进行比对、分析结果显示,该序列属于猴痘病毒分支Ⅱ(西非分支)B.1.3 型。确诊为猴痘病毒感染。结论 猴痘属于新发传染病,根据接触史、临床表现及核酸检测结果可作出诊断。应提高对猴痘临床表现的认识,避免可能发生的漏诊误诊。
A case of monkeypox and literature review
YANG Ligang1, AN Ningbo1, WEN Yunjing2
1.Dermatology Hospital, Southern Medical University, Guangzhou 510091, China; 2.Guangzhou Center for Disease Control and Prevention, Guangzhou 510440, China
Corresponding author: YANG Ligang, E-mail: yanglg3@hotmail.com
[Abstract] Objective To investigate the clinical manifestations, laboratory tests and diagnosis of monkeypox. Methods The clinical and laboratory data of a recently diagnosed monkeypox patient were analyzed, and the data of reported cases were reviewed.Results This case was a 43-year-old male patient with erythema and papules on the pubis and penis 2-3 days after fever. The rashes began with erythema, followed by pustules and ulcers. The patient had a previous history of syphilis. Dermatological examination revealed erythematous swollen pubic mound with pustules and crusts on the right side and a pustule with crust on both the foreskin and the corona of the glans penis. Monkeypox virus nucleic acid test was positive in the skin, blood and throat swab samples. The gene sequence was compared and analyzed using the Nextclade tool (reference genome NC_063383.1), and the results showed that the sequence was consistent with that of monkeypox virus clade II(West African clave), type B.1.3. Monkeypox virus infection was confirmed. Conclusions Monkeypox is an emerging infectious disease, which can be diagnosed according to exposure history, clinical manifestations and the results of nucleic acid test. The awareness of clinical manifestations of monkeypox should be improved to avoid the possible misdiagnosis.
[Keywords] monkeypox; genital
猴痘是一种由猴痘病毒(monkeypox virus)引起的人畜共患的传染病[1],可以在人与人之间传播,也可以通过接触感染的动物传播,甚至可能因为接触有猴痘病毒的物体表面从环境中感染。此前该病在非洲局部流行,近年在非洲以外国家出现局部小爆发[2]。在中国,猴痘属于新发传染病。本文报道新近确诊的1例猴痘患者的临床表现及诊断过程,并与国外报道的病例进行对比,以提高对该疾病的认识,以免误诊。
1 资料与方法
收集南方医科大学皮肤病医院1例在生殖器部位出现脓疱溃疡患者的流行病学资料,记录其发病过程、临床表现及皮肤科检查结果。在皮损及咽喉部位采集拭子标本,并采集患者血液标本,送广州市疾病控制中心及国家疾控中心实验室进行猴痘病毒核酸检测。同时搜索国内外猴痘病毒文献,并与本例患者临床表现及病毒检测结果进行对比分析。
2 结果
2.1 发病经过及临床表现
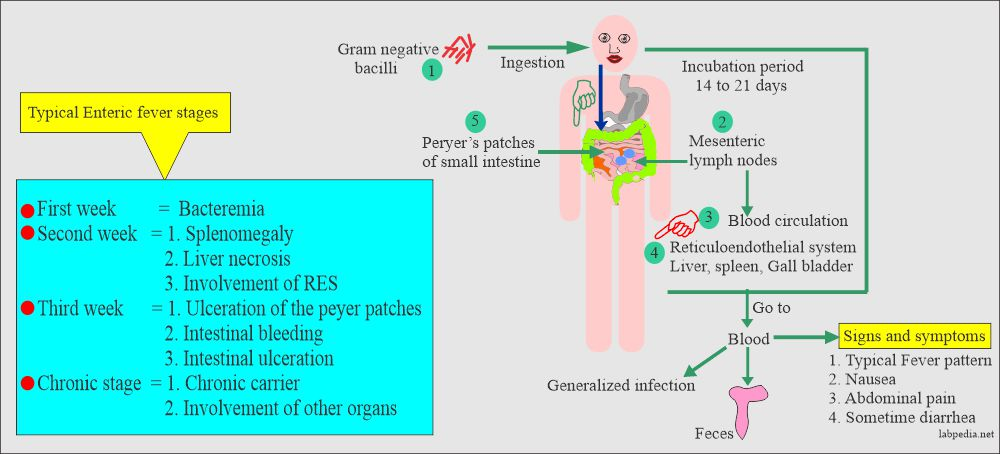
患者男,43岁,中国籍。因阴阜部及冠状沟出现红肿及脓疱1周于2023年6月至我院就诊。就诊前曾出现发热,温度介于39~40 ℃,自服布洛芬退烧。患者3 d前开始在阴阜及冠状沟出现红斑丘疹,阴阜部皮肤红肿。患者2周前有可疑引起感染的接触史。近期无出境史。既往有梅毒史,已正规治疗。天花疫苗接种史不明。皮肤科检查发现患者右侧阴阜部红肿明显,红肿部位可见结痂脓疱,阴茎包皮及冠状沟各1处结痂脓疱。触摸右侧腹股沟淋巴结肿大明显(图1)。
图1 右侧阴阜及阴茎可见伴有痂皮的脓疱
Figure 1 Pustules with crust on the right mons pubis and penis.
2.2 实验室检测结果
患者皮损、咽喉拭子及血液标本行猴痘病毒核酸检测结果显示均为阳性,皮损标本CT值24.85~27.52,咽喉拭子标本CT值36.92~38.14,全血CT值39.4~39.8。利用 Nextclade工具(参考基因组 NC_063383.1)对该序列进行比对、分析结果显示,该序列属于猴痘病毒分支Ⅱ(西非分支)B.1.3 型[3]。
患者人免疫缺陷病毒抗体(HIV)检测阴性, 梅毒快速血浆反应素试验1∶ 2。
2.3 诊断及治疗
结合流行病学史、临床表现、核酸检测结果,诊断为猴痘。患者隔离休息1周后皮损消退。
3 讨论
感染猴痘可出现多种临床症状和体征。感染最初1~5 d,患者可因为病毒血症出现发热、头痛、背痛、肌肉酸痛、乏力及淋巴结肿大[3-5]。发热消退1~3 d后开始出现斑疹、丘疹、脓疱等皮疹。皮疹持续2~3周开始结痂脱皮。传统病例皮疹通常从面部开始,向手掌和脚底延伸,并可累及口腔粘膜、结膜、角膜和/或生殖器。但在一些流行地区,皮损可以最初出现在生殖器部位,并从生殖器部位向其他部位扩散。一些病例仅在生殖器部位出现皮损,并不向其他部位扩散[6]。本例患者皮损也仅限于生殖器部位。
及时和准确的诊断对于控制猴痘的流行是至关重要的。疾病流行早期,医务人员缺乏对猴痘感染的认识,往往错失为可疑病人提供检测的机会[7]。快捷准确的病毒检测对于早期诊断同样是必不可少的。检测采用的标本包括皮损组织液(水疱液)、痂皮、咽喉拭子标本及血液标本。皮损标本因为病毒载量高,核酸检测阳性率高,应作为首选标本[8]。本例患者尽管皮损已开始结痂,但皮损核酸检测结果CT值低于咽喉、血液标本CT值,验证皮损病毒载量高。目前已开发多种猴痘病毒检测方法[9-10],为可疑猴痘病例的诊断提供保障。
轻症无合并症的猴痘患者,通过对症处理,比如使用退烧药,加强皮损部位清洁以预防皮损部位继发感染,加强营养支持,多数病例可自行痊愈。少数有合并症、重症患者需接受综合治疗。目前多国猴痘病例集中在特定人群,因此有必要加强在该类人群中的健康教育宣传。数据显示,感染猴痘的一些病例同时合并包括HIV感染在内的性传播疾病[11],因此对于猴痘病人,同时应加强其他性传播疾病的筛查。
本文所报告患者因生殖器部位皮肤红肿伴脓疱结痂,皮损、咽喉及血液猴痘病毒核酸检测阳性,确诊为猴痘病例。此病例为中国大陆地区学术期刊首次报告的本土感染病例。此病例的诊断有助于提高临床医务人员识别诊断猴痘的警惕性及能力,同时,对该患者感染途径的追踪,对于本地区猴痘病例的监测及控制有非常重要的意义。
[参考文献]
[1]SILVA N I O, DE OLIVEIRA J S, KROON E G, et al. Here, there, and everywhere:the wide host range and geographic distribution of zoonotic orthopoxviruses[J]. Viruses,2020,13(1):43.
[2]KIPKORIR V, DHALI A, SRICHAWLA B, et al. The re-emerging monkeypox disease[J]. Trop Med Int Health, 2022,27(11):961-969.
[3]WHO. Clinical management and infection prevention and control for monkeypox: interim rapid response guidance 2022[S].Geneva:WHO,2022.
[4]BESOMBES C, GONOFIO E, KONAMNA X, et al. Intrafamily transmission of monkeypox virus, central african republic, 2018[J]. Emerg Infect Dis, 2019,25(8):1602-1604.
[5]CICES A, PRASAD S, AKSELRAD M, et al. Mpox update:clinical presentation, vaccination guidance, and management[J]. Cutis, 2023,111(4):197-202.
[6]LEE J, MCLEAN J, ZUCKER J, et al. Mpox genital lesions: a large single center experience with intermediate follow up[J]. J Urol, 2023,9:101097JU0000000000003579.
[7]ZUCKER J. CROI 2023: epidemiology, diagnosis, and management of mPox[J]. Top Antivir Med, 2023,31(3):510-519.
[8]LIM C K, MCKENZIE C, DEERAIN J, et al. Correlation between monkeypox viral load and infectious virus in clinical specimens[J]. J Clin Virol, 2023,161:105421.
[9]CHAUHAN R P, FOGEL R, LIMSON J. Overview of diagnostic methods, disease prevalence and transmission of mpox (formerly aonkeypox) in humans and animal reservoirs[J]. Microorganisms, 2023,11(5):1186.
[10]CORREIA C, ALPALHAO M, DE SOUSA D, et al. Detection of Mpox by PCR from the skin and oropharynx over the course of infection: a prospective study[J]. J Am Acad Dermatol, 2023,7:S0190-9622(23)01014-9.
[11]MITJA O, ALEMANY A, MARKS M, et al. Mpox in people with advanced HIV infection: a global case series[J]. Lancet, 2023,401(10380):939-949.